Focus of this report
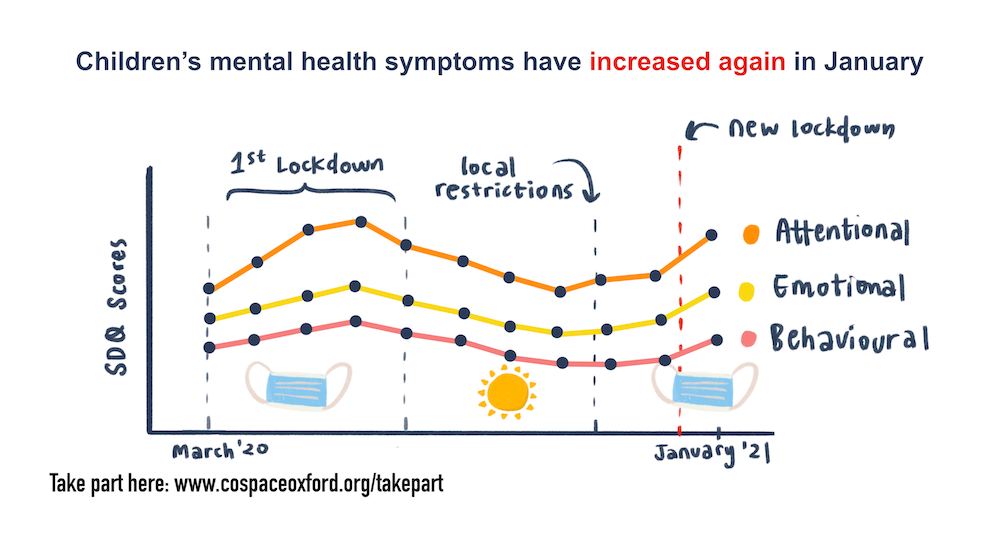
In this report, we focus on the following mental health outcomes as measured by the Strengths & Difficulties Questionnaire (SDQ). This is a well-validated behavioural screening questionnaire. It exists in several versions allowing both reporting by parents/carers (the focus of this report) and self-reporting by adolescents.
To examine ‘caseness’ (see below) we also used the SDQ impact supplement, which assesses the impairment of the identified problems across four domains (the child’s home life, friendships, school-life and leisure activities) and distress. Impact items are scored on a 4 point scale from 0 if either “not at all” or ”only a little”, 1 if “quite a lot” and 2 if “a great deal”. Scores on the impairment and distress items are totalled, leading to a maximum total impact score of 10.
The following subscales were used:
- Behavioural difficulties (conduct problems subscale): items relate to the child doing what they are asked, having tantrums, fighting, lying or stealing things (e.g. whether the child “often lies, or cheats”, or is “generally obedient, usually does what adults request);
- Emotional difficulties (emotional symptoms subscale): items relate to the child being worried, afraid, unhappy, clingy and having physical symptoms of anxiety (e.g. whether the child is “Often unhappy, down-hearted or tearful”, or has “many worries, often seems worried”);
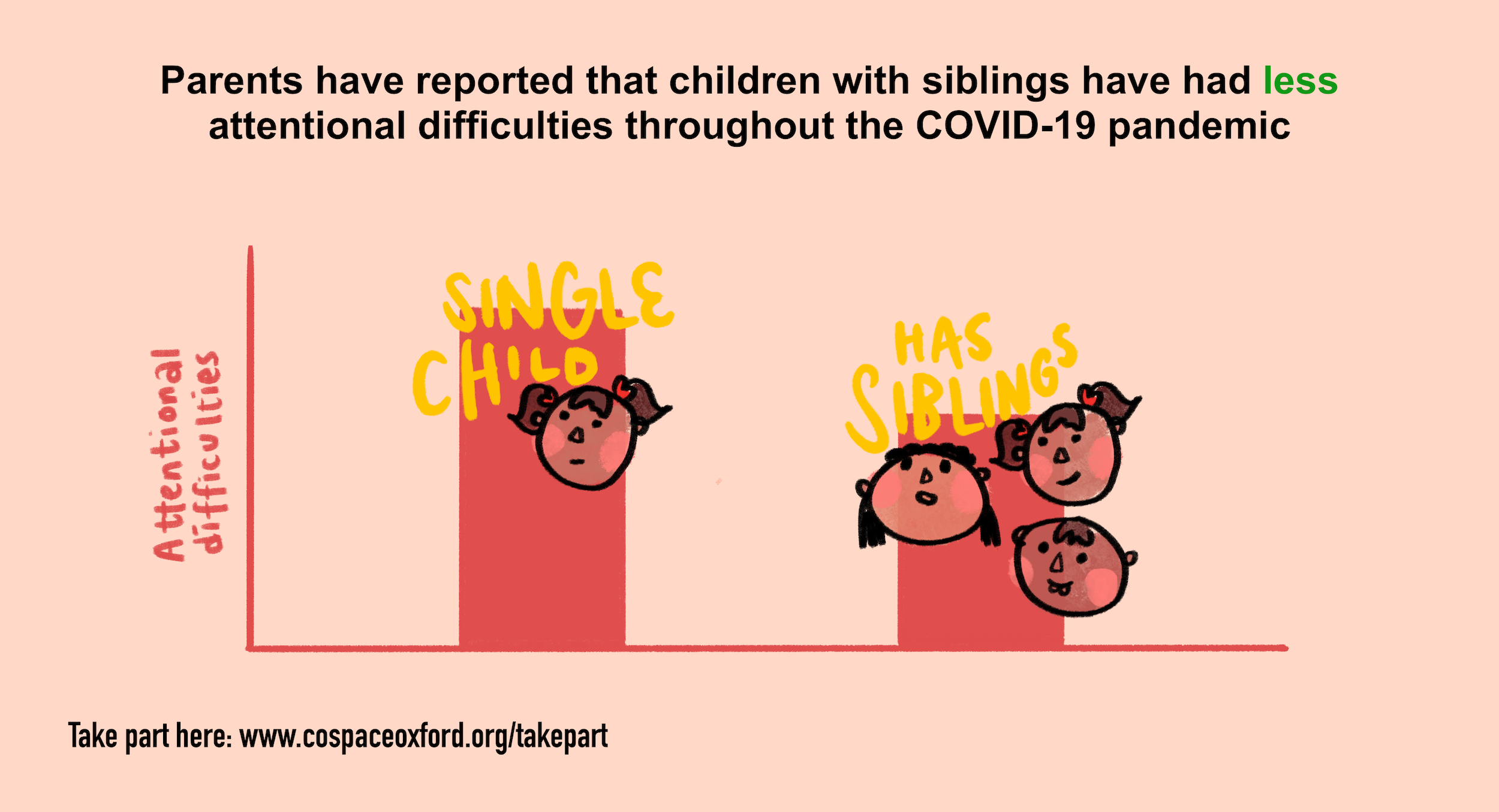
- Restless/attentional difficulties (hyperactivity/inattention subscale): items relate to the child being restless, fidgety, distractible, impulsive and having a good attention span (e.g. whether the child “sees tasks through to the end, good attention span”, or is “restless, overactive, cannot stay still for long”).
Parent-reported behavioural, emotional, and restless/attentional difficulties were looked at in terms of:
- Symptom severity (i.e., continuous SDQ scores) – each subscale consists of 5 items which are summed to compute a total subscale score (ranging from 0-10, with 10 indicating the most severe difficulties).
- ‘Caseness’ (i.e., SDQ scores categorised on the basis of symptoms/interference) – a combination of SDQ symptom score and rated interference in daily life were used to determine the likelihood (i.e., possible or probable) of meeting diagnostic criteria for emotion problems (e.g. anxiety or depression), conduct problems (e.g. conduct disorder or oppositional defiant disorder) or hyperactivity/inattention problems (e.g. Attention Deficit Hyperactivity Disorder; ADHD). In this report, we categorised participants as being either ‘possible’/’probable’ or ‘unlikely’ cases, to err on the side of being inclusive to those who might be a potential ‘case’.
These outcomes were examined for groups based on:
- Age (primary school-aged [4-10 years] or secondary school-aged [11-17 years]);
- Age and gender (primary aged female or male and secondary aged female or male);
- Special educational needs and/or neurodevelopmental differences (SEN/ND or no SEN/ND);
- Household income (more or less than £16,000 per year, i.e., below the poverty line);
- Single adult household (single or non-single adult household);
- Presence of siblings (living with siblings or without siblings).
Key findings
Based on parent/carer reports within the Co-SPACE sample:
- Behavioural, emotional, and restless/attentional difficulties have increased again since the latest national lockdown was introduced in January. This was especially the case in primary school-aged children (4-10 years old).
- More secondary school aged girls than boys had emotional problems in January 2021.
- Children with SEN/ND and those from low-income or single adult households have continued to show elevated mental health symptoms throughout the pandemic, with higher levels of behavioural, emotional, and restless/attentional difficulties.
- Not having a sibling was associated with higher levels of restless/attentional difficulties throughout the pandemic (but was not associated with differences in behavioural or emotional symptoms).